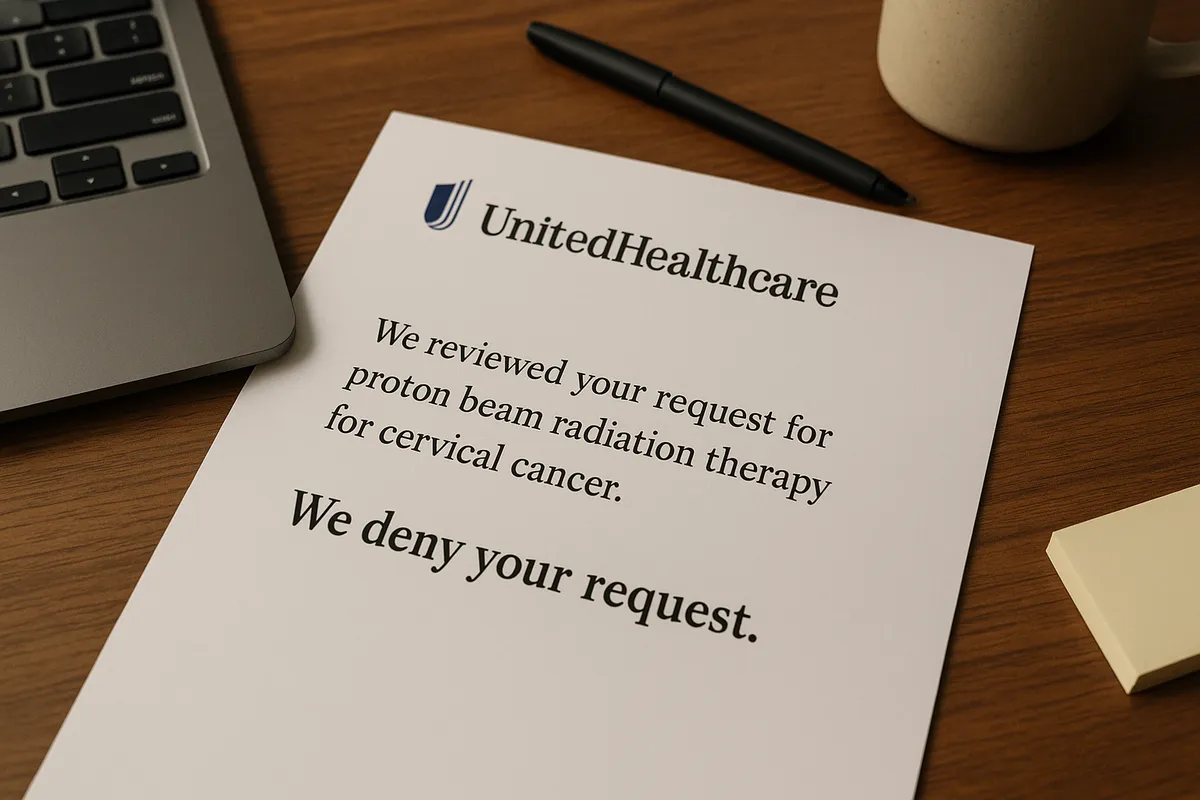
Consumers who were members, participants or beneficiaries of a UnitedHealthcare Insurance Co. or UnitedHealthcare Services LLC employee welfare benefit plan and, between March 26, 2016, and Aug. 28, 2023, they or a covered beneficiary received a denial of a precertification request or post-service benefit claim for proton beam radiation therapy to treat certain cancers may be eligible to claim up to $75,000 from a class action settlement.
UnitedHealthcare Insurance Co. and UnitedHealthcare Services LLC agreed to pay $6.75 million to settle a class action lawsuit alleging it wrongfully denied PBRT coverage for prostate, primary central nervous system, cervical and gynecological cancers.
Who can file a claim?
Class members must meet all of the following criteria:
- They were a member, participant or beneficiary of an employee welfare benefit plan governed by the Employee Retirement Income Security Act of 1974, which UnitedHealthcare Insurance Co. and/or UnitedHealthcare Services LLC administered and/or insured.
- Between March 26, 2016, and Aug. 28, 2023, they or a beneficiary covered by their plan:
- Were diagnosed with one of the following cancers:
- Prostate cancer
- Primary central nervous system cancer
- Cervical or gynecological cancer
- Received a denial of a precertification request or post-service benefit claim for PBRT to treat one of the above cancers for clinical reasons
- Paid out-of-pocket for PBRT treatment after such a denial
- Did not receive payment for the PBRT treatment by any other commercial, self-funded or governmental health benefits payor
If individuals received a notice from the settlement administrator with their name and address as the intended recipient, UnitedHealthcare’s records indicate they may be a class member.
How much can class members receive?
Eligible class members can receive up to $75,000 as reimbursement for out-of-pocket costs paid or still owed for PBRT treatment for the covered cancers. The total settlement fund is $6.75 million. If the total amount of approved claims exceeds the settlement fund, the settlement administrator will reduce each approved claimant’s payment on a pro rata basis.
How to claim a class action payout
To claim an award, class members must submit a claim form with supporting documentation by Oct. 29, 2025. They can submit claims in several ways:
- Complete the online claim form
- Download, print, fill out and mail the PDF claim form
- Email the completed claim form and documentation to the settlement administrator
- Mail the completed claim form and documentation to the settlement administrator
Settlement administrator's mailing address: United PBT Settlement Administrator, c/o Rust Consulting Inc., 8966 PO Box 2599 Faribault, MN 55021-9599, info@UnitedPBTSettlement.com
Is proof or documentation required to submit a claim?
Yes. Claimants must provide documentation to support the amount they claim. Acceptable proof includes:
- Receipts showing payment for PBRT treatment from a hospital, treatment center or physician
- Cancelled checks
- Credit card records
- Documentation from UnitedHealthcare Insurance Co.
- Loan documentation
- Current collection notices
- Unpaid and currently owing invoices or bills from the provider or facility
- Existing self-pay agreements with the provider
To file an online claim, class members must provide the claimant ID number located on the settlement notice they received.
Payout options
The settlement administrator will mail checks to the address eligible claimants provide on their claim form.
Settlement fund breakdown
The settlement fund includes:
- Settlement administration costs, attorneys’ fees and expenses, and service awards to class representatives: Up to $2,500,000 paid separately from payments to class members
- Payments to class members: Up to $6.75 million
Important dates
- Deadline for exclusion: July 28, 2025
- Deadline to file a claim: Oct. 29, 2025
- Final approval (fairness) hearing: Dec. 12, 2025
When is the UnitedHealthcare PBRT settlement payout date?
The settlement administrator will issue payments to qualifying class members after it resolves any appeals and the court grants final approval of the settlement.
Why did this class action settlement happen?
The class action lawsuit alleged UnitedHealthcare Insurance Co. and UnitedHealthcare Services LLC wrongfully denied precertification requests and post-service benefit claims for PBRT for certain cancers. The plaintiffs claimed UnitedHealthcare improperly denied these claims under ERISA-governed plans.
UnitedHealthcare denied any wrongdoing but agreed to settle to avoid the cost, delay and uncertainty of further litigation. As part of the settlement, UnitedHealthcare also agreed to revise its PBRT policy.
.png)







.webp)
.webp)
.webp)

.webp)
.webp)
.webp)
.webp)







.svg)