Update: The Aetna proton beam therapy settlement was granted final approval on Nov. 18, 2025.
Members, participants or beneficiaries of an Employee Retirement Income Security Act of 1974-governed employee welfare benefit plan administered or insured by Aetna Life Insurance Co. who, between Jan. 1, 2015, and March 31, 2024, had themselves or covered beneficiary denied coverage for proton beam therapy to treat localized prostate cancer may qualify to claim $12,000-$48,000 from a class action settlement.
Aetna Life Insurance Co. agreed to pay $3.42 million to resolve a class action lawsuit alleging it wrongfully denied coverage for PBT for localized prostate cancer under certain ERISA-governed health plans.
Who can file a claim?
Class members must meet the following criteria:
- They were a member, participant or beneficiary of an ERISA-governed employee welfare benefit plan administered and/or insured by Aetna.
- They (or a covered beneficiary) were diagnosed with localized prostate cancer.
- They submitted a precertification request for proton beam therapy before the date of service (unless their plan did not require precertification).
- Their precertification request was after Oct. 9, 2020, and they had an intact prostate at the time of the request.
- They received a precertification denial for PBT between Jan. 1, 2015, and March 31, 2024.
- The denial cited terms such as “experimental,” “investigational,” “unproven,” “superior,” “superiority” or “more effective” as the basis for denial (unless these terms were expressly included in their plan’s definition of “medical necessity”).
- They received PBT for the same diagnosis code with no allowed post-service PBT benefit claim(s).
- They had no allowed claims for an alternative recognized medical treatment (excluding treatment plans that included PBT in combination with another modality).
Additionally, the class includes individuals who had a precertification request for PBT that was initially approved but then received a denial of all post-service claims for the same diagnosis code between Jan. 1, 2015, and March 31, 2024, under the same denial criteria as above.
Who is excluded from the class?
- Individuals who received coverage for PBT or for certain alternative recognized medical treatments from another insurance carrier
- Individuals who received a final denial for an administrative reason (such as not being covered under an Aetna plan)
How much is the Aetna Life Insurance payout?
Each eligible class member who submits a valid claim form will receive a minimum payment of $12,000. Those who paid or incurred debt for proton beam therapy treatment totaling more than $12,000 may receive up to $48,000, depending on the documentation they provide.
There are approximately 71 potential class members, and the total settlement fund for class member payments is $3,408,000 (71 x $48,000 = $3,408,000). If fewer than 71 class members submit claims, the remaining funds (except for a $15,000 individual release payment to the lead plaintiff) may be distributed to charitable organizations as designated by the court. Any remaining funds after that will revert to Aetna.
How to claim a class action rebate
Class members can complete the online claim form or download, print and complete the PDF claim form (part of the settlement agreement) and mail or email it to the settlement administrator. All claim forms and supporting documents must be submitted online, emailed or postmarked by Oct. 3, 2025.
Settlement administrator's contact information: Lemmerman v. Aetna Life Insurance Company c/o Atticus Administration PO Box 64053 St. Paul, MN 55164, AetnaPBTSettlement@atticusadmin.com
Class members whose address changes should complete a change of address form to ensure they receive payment.
What information is required to submit a claim?
- To submit an online claim or change of address form, class members must provide their claimant ID and last name.
- To receive more than $12,000 (up to $48,000), class members must provide documentation showing they paid or incurred debt for proton beam therapy treatment above $12,000. Acceptable documentation includes:
- Receipts for PBT treatment from hospitals, treatment centers or physicians
- Cancelled checks or credit card records
- Notarized affidavits or sworn statements from the person who paid (or their authorized representative)
- Loan documents, collection notices, demands for payment or self-pay agreements with the provider
Payout options
Payments will be sent by check to the address provided on the claim form.
$3.42 million settlement fund breakdown
The $3,420,000 settlement fund covers:
- Service award to lead plaintiff: $15,000
- Payments to class members: $3,408,000
Aetna Life Insurance Co. will also pay an undetermined amount of settlement administration costs and up to $1,675,000 for attorneys' costs and expenses. These costs do not affect or reduce class member payments.
Important dates
- Exclusion deadline: Oct. 3, 2025
- Deadline to file a claim: Oct. 3, 2025
- Final approval (fairness) hearing: Nov. 18, 2025
When is the Lemmerman v. Aetna payout date?
If the court grants final approval and there are no appeals, the settlement administrator will mail payments to class members approximately 65 days after the settlement becomes final.
Why did this class action settlement happen?
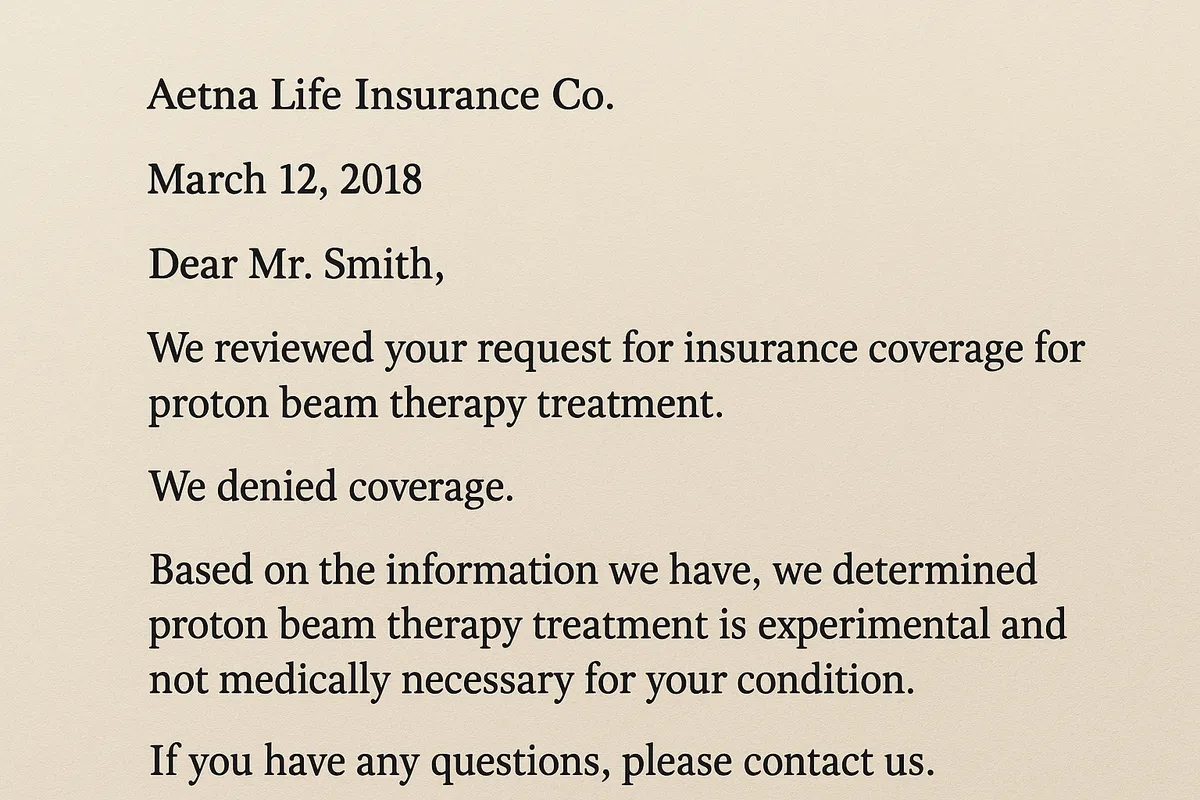
The class action lawsuit alleged Aetna wrongfully denied coverage for proton beam therapy for localized prostate cancer, citing reasons such as the treatment being “experimental,” “investigational” or “not medically necessary.”
Aetna denies any wrongdoing but agreed to settle to avoid the cost, delay and uncertainty of further litigation.
.png)







.webp)
.webp)
.webp)

.webp)
.webp)
.webp)
.webp)







.svg)
Comments